You may wonder about the causes of breast cancer and in particular if the breast cancer gene (BRCA1 or BRCA2) is a factor for you and your family. Angelina Jolie certainly brought this into the limelight when in 2013, she underwent an elective, double mastectomy after testing positive for the gene.
 On the one hand, the gene is a factor for less than 1%1 of women, but on the other hand there are many other factors that come into play including: age, body factors, lifestyle, previous medical conditions and the treatments one has undergone.
On the one hand, the gene is a factor for less than 1%1 of women, but on the other hand there are many other factors that come into play including: age, body factors, lifestyle, previous medical conditions and the treatments one has undergone.
Here’s a good list from Cancer Treatment Centers of America2:
GENERAL
- Aging: On average, women over 60 are more likely to be diagnosed with breast cancer. Only about 10 – 15 percent of breast cancers occur in women younger than 45. However, this may vary for different races or ethnicities.
- Gender: Although nearly 2,000 men will be diagnosed with breast cancer each year, breast cancer is 100 times more common in women. The National Cancer Institute estimates that over 190,000 women will be diagnosed with breast cancer annually.
GENETICS
- Family history: Having a family history of breast cancer, particularly women with a mother, sister or daughter who has or had breast cancer, may double the risk.
- Inherited factors: Some inherited genetic mutations may increase your breast cancer risks. Mutations in the BRCA1 and BRCA2 genes are the most common inherited causes. Other rare mutations may also make some women more susceptible to developing breast cancer. Gene testing reveals the presence of potential genetic problems, particularly in families that have a history of breast cancer. Read about Angelina Jolie’s decision based on her BRCA1 test.
BODY
- Obesity: After menopause, fat tissue may contribute to increases in estrogen levels, and high levels of estrogen may increase the risk of breast cancer. Weight gain during adulthood and excess body fat around the waist may also play a role.
- Not having children: Women who have had no children, or who were pregnant later in life (over age 35) may have a greater chance of developing breast cancer. Breast-feeding may help to lower your breast cancer risks.
- High breast density: Women with less fatty tissue and more glandular and fibrous tissue may be at higher risk for developing breast cancer than women with less dense breasts.
- Certain breast changes: Certain benign (noncancerous) breast conditions may increase breast cancer risk.
- Menstrual history: Women who start menstruation at an early age (before age 12) and/or menopause at an older age (after age 55) have a slightly higher risk of breast cancer. The increase in risk may be due to a longer lifetime exposure to the hormones estrogen and progesterone.
LIFESTYLE
- A sedentary lifestyle: Physical activity in the form of regular exercise for four to seven hours a week may help to reduce breast cancer risk.
- Heavy drinking: The use of alcohol is linked to an increased risk of developing breast cancer. The risk increases with the amount of alcohol consumed.

PREVIOUS TREATMENTS
- Birth control pills: Using oral contraceptives within the past 10 years may slightly increase the risk of developing breast cancer. The risk decreases over time once the pills are stopped.
- Combined post-menopausal hormone therapy (PHT): Using combined hormone therapy after menopause increases the risk of developing breast cancer. Combined HT also increases the likelihood that the cancer may be found at a more advanced stage.
- Diethylstilbestrol exposure (DES): Previous use of DES, a drug commonly given to pregnant women from 1940 to 1971 to prevent miscarriage, may slightly increase the risk of developing breast cancer. Women whose mothers took DES during pregnancy may also have a slightly higher risk of breast cancer.
- Radiation exposure: Women who, as children or young adults, had radiation therapy to the chest area as treatment for another cancer have a significantly increased risk for breast cancer.
Birth Control Link to Cancer
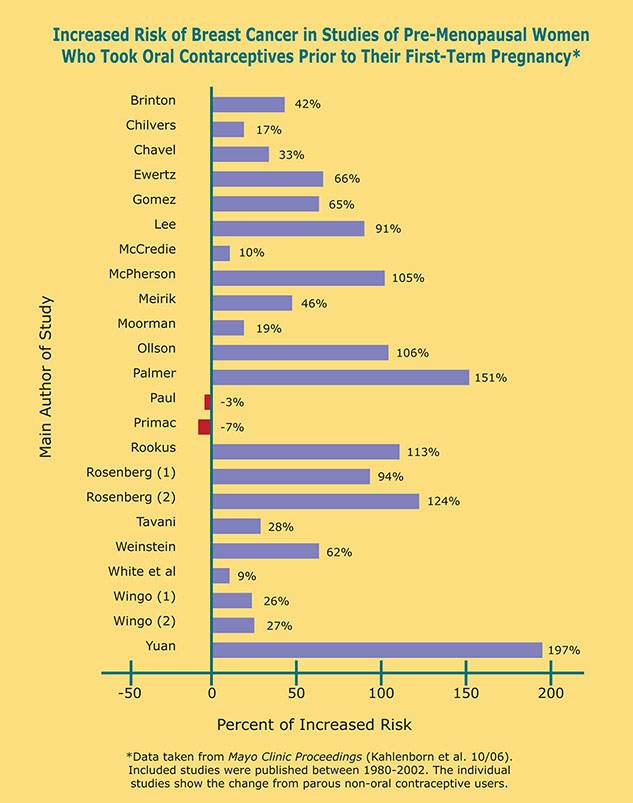
Since breast cancer is the most common cause of death for women in the in the United States for those between the ages of 20-59, there have been numerous studies about it. Twenty three of those studies looked at the possible correlation between birth control and cancer. Of those studies, 21 of them showed that there was a connection and in some studies a very strong connection. Here’s a chart3 showing a comparison:
Also, research studies show that breast cancer risk is increased by almost three times for women who had the “Shot” (Depo-Provera) for 3 years or more before age 25.
A key point is that putting chemicals into one’s body through birth control pills, IUD’s, and the shot is something that you make a decision about – to do this, or not to do this. You can choose to avoid the risk of cancer. Natural Family Planning avoids these risks and is a method to seriously consider. As mentioned above, if a woman has never had children before, the risk for breast cancer is increased and in that caseneeds to take special care of her body.
M. Brady
Disclaimer: The views presented in the above blog article are not necessarily the views of the Birth Control Institute. This article is provided to assist those who desire to do further research.
Footnotes:
